|
Purpose
A new trabeculoplasty procedure, using a selective neodynium (Nd):YAG laser has been developed (1,2) in order to electively target the pigmented trabecular meshwork.
The purpose of this work was to investigate the safety and the efficacy of the method in terms of reduction of the intraocular pressure (IOP).
Population
Fifty-nine eyes of 36 patients were treated. All patients had primary open angle glaucoma (OAG) with IOP uncontrolled by medical therapy. All patients were older than 50 years. Patients selected had no past history of conventional or laser ocular surgery.
Materials and Methods
A Coherent Selecta 7000 TM laser (Coherent Inc, Palo Alto, CA), a frequency doubled Q switched Nd: YAG laser was used for all treatments. The spot size and the pulse duration are : 400µ and 3ns. The operator can vary energy delivered, the starting pulse energy being between 0,8mJ and 1mJ. The power was adjusted to obtain a clinically detectable reaction without frank vaporization bubble . A total of approximately 110 nonoverlapping spots were placed over 360°of the anterior limit of the posterior trabecular meshwork. The IOP was checked at one hour; 2 hours, the following day, one week, 5 weeks, 3 months, 6 months and a year after laser treatment. Minimum follow-up was one year for all eyes.
|
Results
- The average patient age was 66.7 ± 8.7 years. The disease had been dicovered 6.38 ± 5.5 years before laser treatment.
- The average total energy was 85.9 ± 30.6mJ, delivered within 118.9 ± 21.9 spots.
- Preoperative IOP was 25.05mmHg ± 6.3mmHg.
- Post-operative IOP at 3 months, was 16.3mmHg ± 3.8mmHg, the average lowering of the IOP was 32.43 ± 0.14%.
- Post-operative IOP at 6 months, was 16.24mmHg ± 2.8mmHg, the average lowering of the IOP was 32.51 ± 0.17%.
- Post-operative IOP at 1 year, was 15.7mmHg ± 2.4mmHg, the average lowering of the IOP : 33.51 ± 0.14%.
- A transient IOP spike, equal or greater than 5mmHg, and resolving within 24h, was observed in 5 cases.
|
|
|
Table 1 : Results
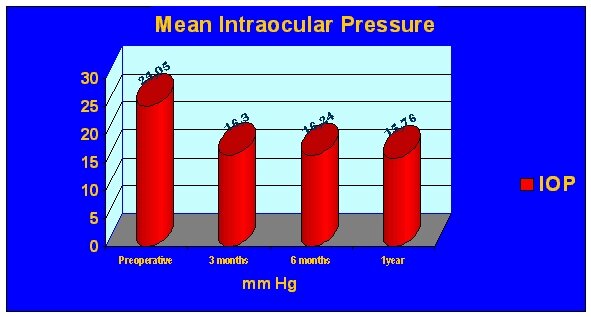
Graph 1: Mean intraocular pressure
Discussion
The study of reference (1) is the in vitro work with the trabecular meshwork by Latina and Park (1995), demonstrating the selectivity of the process. Equipment that we used was developed specifically for trabeculoplasty, combining low treatment energy and short pulse duration, with a wavelength absorbed by melanine. The absence of thermal effect and the limited duration allow a reduction in radiant energy preserving the structural integrity of the meshwork.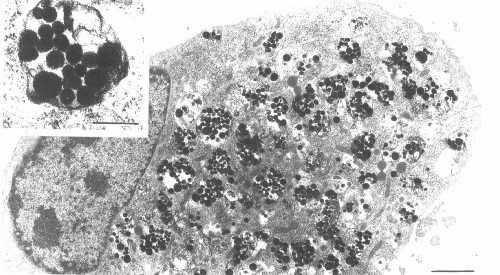
Photograph 1 : ultrastructural image of in vitro pigmented trabecular meshwork cell examined with transmission electron microscopy. Melanine granules are stored in phagozomes (Latina and Park).
Photograph 2 : ultrastructural image of in vitro trabecular meshwork cell 4h after irradiation with strong amount (7 times cellular death threshold) by a switched Q Nd:YAG laser. Lysozomal membranes are broken and melanine is dirupted, whereas the adjacent structures remain intact (Latina and Park).
-
The pilot study (2) using the Coherent Selecta 7000 TM Nd:YAG laser in 31 eyes, showed 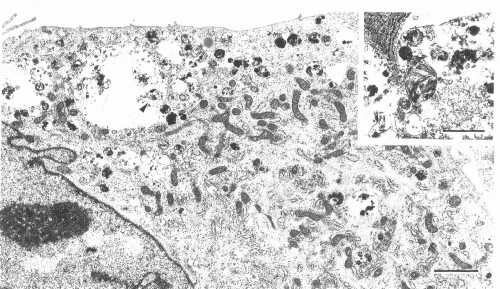 comparable results: 31.6% reduction of the IOP at 1 year and 6 transient pressure elevations resolved in 24 hours. comparable results: 31.6% reduction of the IOP at 1 year and 6 transient pressure elevations resolved in 24 hours.
- In the multicentric study (3) published later, the IOP reduction was 23.5% at 26 weeks.
-
The results published in Japan (4) reported 38.1% IOP reduction at 6 months, with an average fall of 4.4mmHg, in a series of 67 eyes.
Other laser techniques
-
The series published on 1983 by Moulin and Haut (5) of trabeculoplasty using the argon laser showed 9.3mmHg average reduction of the IOP at 15 months including patients older than 60 years. The results obtained using selective laser trabeculoplasty are equivalent in our study.
-
Mermoud et al. (6) published in 1992 results at 3 months showing 32.9% IOP fall using the argon laser and 24.5% using a Nd:YAG laser.
-
The diode laser is also used for the trabeculoplasty, but the results at 3 months showed 2.4% IOP drop using this laser and 30% using the argon laser (7).
Graph 2 : Percentage of IOP lowering
Conclusion
|
Selective laser trabeculoplasty (SLT) appears to be a safe and effective technique to lower the intraocular pressure, and could be an alternative to argon laser trabeculoplasty.
Larger series and longer follow-up comparing SLT to standard ALT are required to know if this techniques should be considered the laser procedure of choice for treatment of open angle glaucoma.
|

|
References
-
M.A.Latina, C.Park Selective Targeting of Trabecular Meshwork Cells : In Vitro Studies of Pulsed and CW Laser Interactions Exp. Eye Res. 1995 ;60/4 :359-372
-
M.A.Latina, S.A.Sibayan, F.Gil-Carrasco, O.Garza-Saide, D.H.Shin, R.J.Noecker Selective Laser Trabeculoplasty :A Pilot Clinical Trial ARVO 1997
-
M.A.Latina, S.A.Sibayan, , D.H.Shin, R.J.Noecker, G.Marcellino Q-switched 532-nm Nd:YAG Laser Trabeculoplasty (Selective Laser Trabeculoplasty) - A Multicenter, Pilot, Clinical Study Ophthalmology 1998;105:2082-2090
-
K.Kano, Y.Kuwayama, S.Mizoue, N.Ito Clinical results of selective laser trabeculoplasty Nippon Ganka Gakkai Zasshi 1999;103/8:612-618
-
F.Moulin, J.Haut Results of argon laser of 100 eyes with open-angle glaucoma (trabeculoplasty, trabeculoretraction) J Fr Ophtalmol 1983;6/8-9:661-670
-
A.Mermoud, C.P.Herbort, C.C.Schnyder, N.Pittet Comparison of the effects of trabeculoplasty using the Nd-YAG laser and the argon laser Klin Monatsbl Augenheilkd 1992;200/5:404-410
-
J.A.Englert, T.A.Cox, R.R.Allingham, M.B.Shields Argon vs diode laser trabeculoplasty Am J Ophthalmol 1997;124/5:627-631
|
|
